Decoding Dysautonomia Part 4: Active Episode Support and Symptom Management
Build your own Flare-up First Aid Kit
There was a time when every flare felt like a setback I couldn’t control. The racing heart, chest pain, tremors, and crushing fatigue made it feel like my body was stuck in survival mode.
But I’ve learned that symptom flares, while unpredictable, are not unmanageable. And each one offers a chance to listen, adjust, and respond with more targeted support.
In this part of Decoding Dysautonomia, I’ll share the tools that helped me weather the storm of symptom flares, and how you can build your own Flare-Up First Aid Kit to support your body when it needs it most.
Whether you’ve been following the series or are just joining now, this part is all about real-time support when your symptoms surge and how to feel less powerless in those moments.
Active Episode Support
When I first began navigating chronic illness, my episodes could last for hours, sometimes even days. Over time, by using many of the strategies I’ll share in this article, I was able to shorten them significantly. Not only that, but the frequency also dropped: from almost daily, to weekly, to once or twice a month—and now, I’ve been flare-free for over six months. That shift has completely changed my quality of life. I’m picking up old hobbies like going to the gym, taking barre classes, and even inverted exercises like trapeze yoga and aerial—activities I never thought I’d be able to return to. I finally feel like I’m back in the driver’s seat of my health.
For many people living with long COVID related dysautonomia, the foundational strategies discussed in Part 3 help lay the groundwork for healing. But while that process unfolds, we also need practical tools to manage symptoms when they arise. Creating a personalized Flare-Up First Aid Kit (your go-to strategies for in-the-moment support) can help you feel more prepared and in control during challenging episodes
Flare-ups can be deeply frustrating. They disrupt your routine, derail your plans, and can make it feel like all your progress has vanished in an instant. But the goal of episode support isn’t to eliminate symptoms entirely—it’s to reduce their intensity, duration, and impact, so you can spend less time in crisis mode and more time living.
The right support strategies will depend on your specific type of dysautonomia and the underlying factors driving your symptoms. That’s why this approach needs to be personalized. But wherever you are in your journey, there are tools that can help.
And above all, please remember: your symptoms are real. While they make this condition so devastating, they are also your body's way of communicating. Symptoms are messages—signals of underlying imbalances that need attention.
Medical Disclaimer
This article is for informational purposes only and is not intended as medical advice. Dysautonomia and long COVID are complex conditions that require individualized care. Always consult your healthcare provider before making changes to your treatment or lifestyle.
Nutrition
If you’ve read Part 1, you know that dysautonomia isn’t a one-size-fits-all condition. It includes multiple types—like POTS (and its many subtypes), Orthostatic Hypotension (OH), Vasovagal Syncope (VVS), and others—each driven by different mechanisms. That means there’s no single protocol for managing flare-ups. What works for one person may not work for another.
To complicate things further, many people experience overlapping symptoms or multiple subtypes at once, making it hard to predict which tools will actually help in the moment. In these situations (especially during an active episode) having strategies that can help calm the autonomic chaos is everything.
Below, I’ll walk through what’s worked for me and many others navigating dysautonomia flares.
Hydration & Electrolytes in Dysautonomia: A Step-by-Step Guide
Managing dysautonomia, especially during flares, requires a solid understanding of how hydration and electrolytes support your autonomic nervous system. Let’s walk through what that actually looks like, one step at a time.
What Electrolytes Do in the Body
Electrolytes are electrically charged minerals that help regulate countless processes in the body. When it comes to fluid balance, you can think of them as traffic directors for your cells—guiding water in and out, helping to maintain blood volume, and keeping tissues properly hydrated.
But their responsibilities don’t stop there. Electrolytes like sodium, potassium, magnesium, and calcium also help your nerves communicate, your cells produce energy, and your muscles contract (including the heart).
Each electrolyte comes with its own job description—like a tiny specialist on your body’s internal team:
🧂 Sodium – The hydration coordinator.
Manages fluid balance and regulates blood pressure by directing where water should go.
🍌 Potassium – The electrical technician.
Keeps your heart rhythm steady and helps nerve signaling and muscles (even your gut!) contract and function smoothly.
🌿 Magnesium – The project manager.
Involved in over 300 enzymatic reactions, including those required for producing energy and calming the nervous system.
🦴 Calcium – The structural engineer.
Helps muscles contract properly, supports nerve signaling, and plays a role in blood clotting and bone strength.
Many of us with dysautonomia are operating with an understaffed electrolyte crew. When any of these are running low, things can feel off and your body starts working less efficiently.
Why Electrolytes Matter in Dysautonomia
In dysautonomia the autonomic nervous system does not properly regulate blood pressure, heart rate, or fluid balance. This dysregulation can be triggered by changes in posture (like moving from lying down to standing), leading to symptoms like lightheadedness, fatigue, tachycardia, and even fainting.
So why are electrolytes such a core piece of managing these conditions? Because they directly support the systems that are impaired:
They help expand blood volume, which can improve circulation and prevent the dramatic blood pressure drops seen in many types of dysautonomia.
They regulate nerve impulses, which are key to autonomic signaling.
They support cardiac function, especially in preventing arrhythmias and erratic heart rate.
They are involved in cellular energy production, helping reduce fatigue and brain fog (particularly supportive for the chronic fatigue flavor of dysautonomia/ long COVID).
Routine blood work is important for monitoring electrolyte levels—and stabilizing electrolytes is one of the most accessible tools we have to help manage symptoms and reduce flares.
Fluid Intake
Many people with dysautonomia benefit from higher-than-average fluid intake to support blood volume. There’s no one-size-fits-all recommendation for fluids, but many individuals with dysautonomia benefit from 2-3 liters (or more) per day. However, it’s always best to follow the guidance of your provider.
Instead of chugging large amounts all at once, aim to drink consistently throughout the day. One simple but helpful habit is starting your morning with a glass of water before getting out of bed. For those that struggle with dizziness upon standing, this small habit can help stabilize blood pressure and make it easier for your body to handle the shift from lying down to standing.
And don’t underestimate the power of hydration rituals. Whether it is having an emotional support water bottle you take everywhere (mine’s an Owala), making electrolyte rich mocktails with sparkling coconut water, bone broth hot chocolate, sleepy girl mocktails with magnesium powder before bed, or even something as simple as drinking a glass of water with a sprinkle of salt first thing in the morning—hydration can be both functional and comforting.
If you're into the idea of fun hydration recipes, I’d be happy to share some of my favorites in a future post. Let me know in the comments!
Fluid Balance
When it comes to dysautonomia, all electrolytes matter—but sodium and potassium often play the biggest roles in fluid balance and how we feel day to day. In this article, we’ll focus on these two in greater detail to help you better understand how they support your body and why they’re so central to symptom management.
🧂 Sodium
Sodium is often the cornerstone of fluid and electrolyte support in dysautonomia, especially in subtypes like hypovolemic POTS, OH, or VVS, where low blood volume is a central issue. When sodium intake increases, it helps the body hold onto water, effectively expanding blood volume and improving blood flow to the brain and heart.
For many people, increasing daily sodium to 3,000–10,000 mg can make a noticeable difference in how they feel. But here’s the catch: this strategy isn’t for everyone—and it definitely isn’t a blanket recommendation. I always look at the full picture first, including a client’s blood pressure history, medications, and any underlying heart or kidney conditions before suggesting an aggressive sodium approach.
And then there’s Hyperadrenergic POTS. This subtype is different. Instead of low blood volume being the main problem, it’s characterized by an overactive sympathetic nervous system—think “fight or flight” mode stuck in the “on” position. In these cases, too much sodium can actually make things worse by driving blood pressure even higher. So again, personalization is key.
One thing I always emphasize (regardless of sodium intake) is including plenty of potassium-rich foods to support electrolyte balance and cardiovascular function.
🍌 Potassium
While sodium often takes center stage, potassium is just as vital—especially for anyone managing long COVID or dysautonomia. Like we talked about earlier, this electrolyte supports nerve conduction, muscle contraction, and cellular hydration. It helps maintain rhythm in your heartbeat and works in tandem with sodium to regulate fluid balance.
Low potassium (hypokalemia) can lead to fatigue, muscle weakness, irregular heartbeat, and worsen tachycardia episodes. During my first major flare, I ended up with hypokalemia. Since then, potassium-rich foods became a non-negotiable part of my routine—and I built my own "flare-up first aid kit" around them. Coconut water has been my go-to anytime I feel a flare coming on, so I always keep some on hand.
I don’t typically recommend potassium supplements unless medically supervised—instead, I guide my clients with a food-first approach. That includes options like:
Coconut water
Avocados
Potatoes
Leafy greens (especially spinach)
Beans and lentils
Oranges and bananas
Regularly getting enough of these electrolytes is key for day-to-day stability and may help reduce the frequency or intensity of flares. In my own experience, I’ve found it helpful to think about electrolyte needs in two categories: what I need for daily maintenance and what I reach for during a flare. During those flare-ups, the demand for sodium and potassium can spike—so my approach shifts depending on how I’m feeling. Let’s explore this idea a bit more.
Flare-Up Support vs Daily Maintenance
During flares, high-sodium electrolyte packets that provide 500-1,000 mg of sodium per serving can help quickly expand blood volume and ease symptoms like dizziness, fatigue, or a racing heart. I typically recommend these concentrated formulas for acute support—but for those with hypovolemic POTS, they may also be essential for daily maintenance, not just flare-ups. This subtype often requires higher sodium and fluid intake overall to manage chronically low blood volume. That said, not everyone needs this level of support for daily maintenance—I didn’t in my own journey. It’s a reminder that what works is highly individual.
Interestingly, electrolytes that include a small amount of sugar can also be beneficial during flares, since glucose helps enhance sodium and water absorption in the small intestine. A few grams of sugar can go a long way here—nothing excessive.
For daily maintenance, I personally did well with some variation of:
Salting food consistently
Drinking electrolyte-rich beverages
Using electrolyte packets with 250–500 mg of sodium per serving as needed
Daily electrolyte needs can fluctuate, so adjusting your intake based on how you’re feeling or what your day looks like, like increased symptoms or physical activity, may be more realistic than sticking to a fixed amount. As always, finding what works takes some trial and error, ideally with guidance from a provider familiar with dysautonomia.
I often get asked which electrolyte packets are best. If that’s something you're curious about, let me know—I’m planning a separate comparison post with a full breakdown of brands and formulations.
When Flares Escalate: The Role of IV Support
In some cases of long COVID and dysautonomia, especially POTS, the low blood volume, dehydration, and electrolyte imbalances that accompany the condition can become severe. When this happens, IV fluids may be used in clinical settings to help stabilize the patient.
Beyond acute use, intermittent saline infusions have also been studied as a supportive therapy. One study found that they led to significant improvements in symptoms and quality of life for individuals with POTS. More recently, a small but growing number of clinicians have explored the use of scheduled saline infusions, such as weekly IV therapy, as a strategy for individuals with more severe or treatment-resistant symptoms of POTS and long COVID. While not a universal solution, some patients have reported meaningful benefits, and it remains an area of interest within ongoing clinical care and research.
While hydration plays a central role in managing symptoms, nutrition (particularly how and when we eat) can be just as impactful for many people.
Meal Timing and Composition
Ever notice your heart racing or your symptoms spiking after a big meal? You’re not imagining it—what and when you eat can have a big impact on how you feel.
For many people with dysautonomia, especially those with POTS or VVS, adjusting meal patterns can be a helpful tool for symptom management. One simple but effective strategy is to opt for smaller, more frequent meals instead of large ones.
Digestion takes a surprising amount of energy. After a big meal, your body redirects blood flow to the digestive tract to help break down and absorb nutrients. That shift can reduce the amount of blood returning to the heart, due to something called splanchnic pooling—blood collecting around organs like the stomach and intestines. For people with POTS, the body compensates for this drop in blood pressure by kicking the heart rate into overdrive, which can intensify symptoms.
Foods to Approach with Caution
While smaller, balanced meals can support more stable blood pressure and circulation, certain foods and beverages may have the opposite effect—triggering or worsening dysautonomia symptoms for some individuals. Responses are highly individualized, but these are common culprits worth considering:
🍷 Alcohol
Alcohol acts as a vasodilator, widening blood vessels and lowering blood pressure (at least initially). It’s also a diuretic, promoting fluid loss and contributing to dehydration and reduced blood volume. These combined effects can intensify symptoms, which is why many people with dysautonomia find it helpful to minimize or avoid alcohol.
☕ Caffeine
Caffeine is a bit of a wildcard. Some people in the dysautonomia community find it helpful for increasing blood pressure, while others have found it can quickly trigger severe flares. Personally, caffeine has been a major trigger for me. I can usually tolerate small amounts from chocolate or certain teas, but stronger drinks like coffee or matcha often lead to tachycardia episodes. This sensitivity may be due to how caffeine stimulates the nervous system, compounding an already heightened sympathetic response. It’s a reminder of how individualized dysautonomia management truly is.
🍞 High-Carbohydrate Meals
Remember when we talked about how digestion redirects blood flow to the gut? Studies have shown that meals high in carbohydrates can worsen this post-meal splanchnic pooling, making symptoms more likely to flare. I started to notice this pattern when heavier, carb-rich meals left me with a racing heart, chest pain, and fatigue afterward. That same splanchnic pooling seemed to be at play here. Once I made that connection, I began approaching meals more strategically. During the peak of my symptoms, I shifted to a lower carbohydrate diet. As someone who loves carbs, this wasn’t an easy change—but it eliminated my post-meal flares. For those experiencing frequent symptom spikes after eating, experimenting with meal composition (especially carbohydrates) may be a helpful place to start.
Balancing Blood Sugar ⚖️
And while we’re on the topic of carbohydrates and meal composition, let’s also briefly talk about the importance of balanced blood sugar in dysautonomia management. You might be wondering—what does blood sugar have to do with a nervous system disorder? As it turns out, blood sugar and dysautonomia are more interconnected than you might think.
During a dysautonomia flare, the nervous system can become hyper-reactive, triggering a “fight or flight” (sympathetic) response. As part of this reaction, the body releases glucose into the bloodstream to provide quick energy for the perceived threat. But without an actual physical demand for that glucose—like running or fighting—that surge can lead to blood sugar instability over time.
Keeping blood sugar steady throughout the day is one important way to support nervous system balance and reduce the frequency and intensity of flares.
For practical strategies on balancing blood sugar, see my article: Decoding Dysautonomia Part 3: The Foundational Strategies.
Once you've tackled meals, another helpful strategy is compression—research shows it can reduce blood pooling and support symptom relief in POTS.
Compression options include:
Waist-high compression garments: These offer full support to both the legs and abdomen, promoting better venous return and minimizing blood pooling in the lower body and abdominal region.
Abdominal binders: These target the abdominal area specifically, helping reduce post-meal splanchnic pooling.
Compression socks: These are typically knee-high and best for addressing blood pooling in the lower legs. While they don't support the abdomen, they can still be helpful for some POTS people during long periods of standing or sitting.
Compression isn’t a fix-all, but for those dealing with symptoms related to blood pooling, it can be a helpful tool to weave into a broader support strategy. There are several additional lifestyle approaches that can help manage dysautonomia symptoms throughout the day.
Lifestyle Support
Living with dysautonomia often requires layering in daily strategies that help support your nervous system and maintain more stable blood flow. Here are a few key tools to keep in mind:
Postural Adjustments
For individuals with POTS, many symptoms are triggered by changes in posture — especially moving from lying down (supine) to standing. Breaking these positional changes into stages can help minimize flares. Start by slowly sitting up, allowing your body time to adjust before moving to a seated upright position. Pause here for a few minutes before attempting to stand. Giving the cardiovascular system time to adapt at each stage can help reduce symptom flares.
If a flare occurs, moving back to a supine position can help restore blood flow to the brain and may prevent loss of consciousness.
♿ Tip: Sitting during activities like showering can also make a difference, especially since heat and standing for long periods are common triggers for those with dysautonomia. Using mobility aids like the shower chair or sitting on the shower floor can provide additional support.
Breathing Techniques
Breathwork might seem simple, but it can be a powerful way to support the nervous system—especially during a flare. Certain breathing techniques help activate the parasympathetic branch of the nervous system, making them useful tools to calm the body when in crisis mode.
Here are a few techniques I’ve found especially helpful:
Diaphragmatic breathing: Also known as “belly breathing,” this method encourages deeper, slower breaths using the diaphragm rather than the chest. Try placing one hand on your stomach and the other on your chest. As you inhale through your nose, your stomach should rise while your chest stays relatively still. Exhale slowly through your mouth. Practicing this regularly can help stabilize the heart rate and blood pressure during flare ups.
Box breathing: This is one of my go-to techniques when I sense an episode coming on. It’s a simple, structured pattern: inhale for a count of four, hold for four, exhale for four, and hold again for four. This rhythmic breathing style can reduce sympathetic nervous system activity.
Pursed-lip breathing: If you ever feel short of breath or lightheaded during a flare, this technique can be especially grounding. Inhale gently through your nose, then exhale slowly through pursed lips, like you’re blowing through a straw. Aim for your exhale to last about twice as long as your inhale. This helps slow both breathing and heart rate, giving your nervous system a chance to recalibrate.
Vagus Nerve Stimulation
Stimulating the vagus nerve can encourage parasympathetic activity and help counter the sympathetic overactivation that often accompanies dysautonomia flares. Fortunately, there are simple, gentle ways to do this. Activities like humming, singing, or chanting create vibration near the vagus nerve, which can trigger a calming response. Mindfulness practices, meditation and slow, intentional breathing can also help support vagal tone and promote relaxation.
Another technique to be aware of is the Valsalva maneuver—a breathing method where you exhale forcefully against a closed airway (typically by closing your mouth, pinching your nose, and trying to exhale out as if blowing up a balloon). While this is sometimes used diagnostically, it can also be helpful for bringing down a racing heart during episodes of tachycardia.
⚠️ Important: The Valsalva maneuver isn’t appropriate or safe for everyone. Always talk to your doctor before attempting this technique, especially if you have underlying heart conditions or other health concerns.
Learning to use the Valsalva maneuver has been one of the most helpful tools for managing my dysautonomia episodes. When my heart rate spikes, it often helps me return to baseline more quickly. It took some time and guidance to learn how to do it properly, but it’s made a noticeable difference in how I manage flares.
Wearables & Health Tracking
Tuning Into the Body’s Signals
Living with a chronic illness often teaches you to become fluent in the body's subtle signals — but truly honoring those signals and making adjustments before they escalate into full flares can be one of the hardest challenges. This ability, called interoception, is your internal sense of things like heart rate, fatigue, blood sugar fluctuations, and more. It's a skill that tends to strengthen over time, especially with practice and self-tracking.
Tools like wearable devices and symptom tracking apps can help build this awareness. They offer objective data points that, when paired with tuning into your own felt experiences, can make it easier to catch early signs of dysregulation. Tracking also helps identify patterns and potential triggers, empowering you to respond more proactively rather than reactively.
Helpful tools include:
⌚ Apple Watch + TachyMon App – A helpful combo for real-time heart rate tracking and alerts. TachyMon is especially useful for catching heart rate spikes and monitoring trends relevant to POTS.
🏃🏽♀️ Fitbit - Great for general heart rate and sleep tracking. While not compatible with TachyMon, it’s a solid entry-level tool for daily monitoring.
💍 Oura Ring - Best for tracking sleep quality, heart rate variability (HRV), and general stress patterns. It’s less effective for monitoring sudden heart rate changes and requires app access to view data, which might be less ideal for those needing quick info on-the-go.
🫀 KardiaMobile 6L EKG - A portable, FDA-approved EKG device for tracking heart rhythm and rate. During the early stages of my symptoms, each tachycardia episode felt overwhelming and scary, and my health anxiety was at an all-time high. Having this device gave me peace of mind and reliable data to share with my providers.
📝 Notes App / Journal - A simple but powerful tool for logging symptoms, flares, and patterns. It can be really helpful for spotting connections over time—and the best part is, many of us already have something like this on our phones or at home. This was actually the very first thing I started doing when I began my dysautonomia journey. I recommend jotting down details like the date and time of flares, what you were doing beforehand, any food or drinks consumed, symptoms experienced, and how long they lasted.
📱 Human Health: Chronic Illness App - Though I haven’t personally used it, this app can organize symptoms, medications, and more for people who want a structured approach to tracking.
🧠 Lumia wearable - This emerging tech tracks blood flow to the head by detecting arterial blood flow signals via shining infrared light at a shallow artery in the ear. For people with dysautonomia, drops in cerebral blood flow can trigger symptoms like lightheadedness and fainting. While more research is underway, this device may offer helpful insights for those trying to better understand and manage their flares.
🩸 Continuous Glucose Monitors (CGMs) — While I would recommend first implementing nutrition and lifestyle strategies to balance blood sugar, these can be helpful for identifying food-related patterns and making targeted changes. CGMs are not essential for most people with dysautonomia, but can be a useful tool if blood sugar swings contribute to symptoms.
Disclaimer: I’m not affiliated with or sponsored by any of the products mentioned here. These are tools I’ve either personally used during my own dysautonomia journey or discovered through research.
Avoiding Common Triggers
Everyone’s triggers can look a little different, but there are a few that tend to show up across the dysautonomia community. Being mindful of these may help reduce the risk of flares:
☕ Caffeine
🍷 Alcohol
🌿 Cannabis
💊 Stimulant medications
🏋️♀️ Intense or prolonged exercise
🌡️ Heat exposure
😥 High stress levels
This is a big topic that deserves a more detailed breakdown, but this article is already packed with information—so I’ll save that for another time. If you’d be interested in a future post exploring common triggers (and how to manage them), let me know!
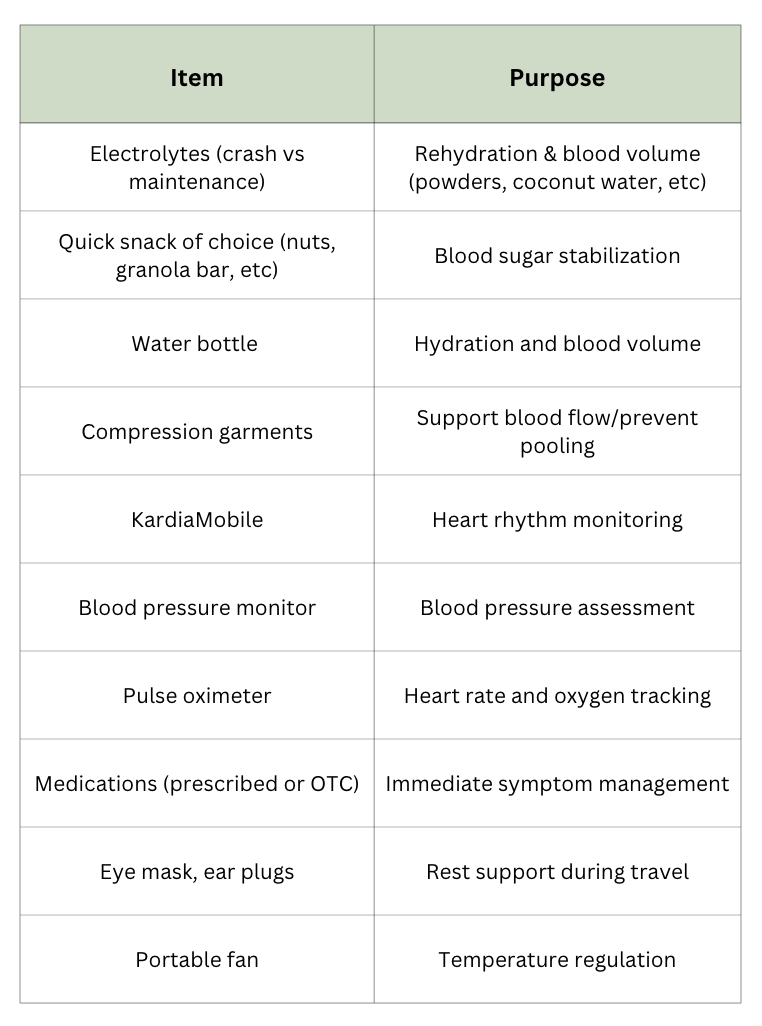
Flare-Up First Aid Kit
Remember that flare-up first aid kit we mentioned earlier? Now’s the time to build it out. And the good news is: it doesn’t have to fit in a box (though it can if you want it to). Your kit can be both mental and physical—a mix of tools, strategies, and comfort items that help you feel more grounded and supported when symptoms spike.
🧠 The Internal Kit: Tools You Can’t See, But Definitely Feel
Think of this as your flare-up menu—a collection of calming strategies you can mentally reach for when things start to go sideways. Reflect on what resonated with you throughout this piece and your own lived experience. Maybe it’s a breathing technique you’ve practiced, a form of vagus nerve stimulation that helps you reset, a comfort show / music to help distract you or calm the nervous system, or simply knowing when to slow down and rest when you notice the beginning signs of a flare.
Your menu might look totally different from someone else’s, and that’s the point. It can be helpful to jot these strategies down in one place so you’re not scrambling to remember what helps when your brain is in full dysautonomia-mode.
✅ Tip: Practicing your go-to tools when you’re not in a flare can help them feel more instinctive when you are.
🎒 The Physical Kit: Tools You Can Toss in a Bag
Here’s where we get tangible. These are the grab-and-go items that can offer real-time relief and support. You might keep a full version of your kit at home and smaller versions in your purse, car, or gym bag for backup on the move.
✅ Tip: Tailor your kit to your most common flare triggers—and where you tend to be when they happen (home, work, gym, traveling, etc).
Buy Me a Coffee ☕ (Decaf, of course)
I want to keep this series free and accessible to the chronic illness community. Living with long COVID and dysautonomia can be financially draining, and for many of us who are partially or fully disabled, accessing support and care can feel out of reach.
If you’ve found this series helpful and you have the means to contribute, I’ve set up a Buy Me a Coffee page—a virtual tip jar where you can make a small donation if you'd like.
Your support helps make it possible for me to continue pouring time, research, and lived experience into creating these resources
Whether you’re able to contribute or not, I’m so grateful you’re here. Thank you for being part of this community. 💛
Wrapping Up
Living with dysautonomia can feel like riding out a storm without a forecast. But with the right tools, strategies, and support, it is possible to find steadier ground. I hope this guide has helped you feel more equipped, empowered, and seen in your journey.
In the final part of this series, we'll shift our focus from symptom management to exploring potential underlying drivers of long COVID-related dysautonomia. While many questions remain, research is growing every day—and with it, new insights and possibilities.
Stay tuned for Part 5, where I’ll share ways to begin uncovering the root causes, along with advanced protocols and next-level strategies that helped support my own recovery process.
And if you’re still in the thick of it, my hope is that this helps bring more sunny days for you ahead.





Another comprehensive post, thank you. I seem to have the high blood pressure symptoms with raised heart rate every time I stand and sit with my feet on the floor (although not as bad). I use the visible wearable and try to keep within my envelope of energy limits. But some days I just have to do things!!
Another great piece. I particularly liked the breakdown of the role each electrolyte playa in the body. I'd definitely appreciate tips/recommendations for choosing electrolyte packets. And I've shared this post with others!